There are federal regulatory standards that nursing homes must meet for providing qualified registered nursing staff. According to McKnight’s.com, fully three-quarters of nursing homes seldom meet the federally registered nurse (RN) staffing level guidelines. In particular, on the weekends, nursing homes are often understaffed, or staff is not there at all according to data gleaned from a year’s worth of payroll data as assessed by Harvard and Vanderbilt medical schools.
The research further shows that 70 percent of the nursing home facilities were reporting higher totals of direct staffing using the CASPER system which communicates with the Centers for Medicare and Medicaid Services (CMS) than in new standard known as Payroll-based Journal (PBJ). Discrepancies were most evident at for-profit nursing homes, then non-profits, and finally government-run facilities.
The study results may have broader implications than just numbers about staffing. How do healthcare outcomes differ with limited or non-existent RN staff? Who handles triage in the nursing home facilities deciding who gets available care and who has to wait? Is there an increase in adverse events such as medication errors or falls when there is a reduced staff?
Most of the data that Medicare is reporting by Nursing Home Care relies on self-reporting of quality measures by nursing home facilities. The data reported can be incomplete, or biased as CMS oversight cannot audit every nuance of care and typically goes for more significant and more prevalent issues. An increase of auditing quality measure reporting is necessary to improve not only the data but enforcement of federal guidelines designed to protect nursing home residents.
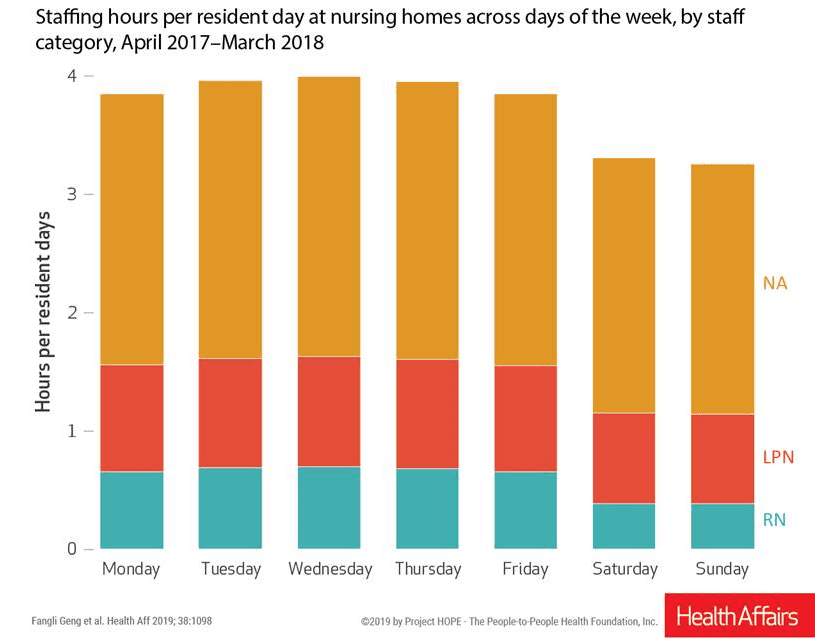
The newer payroll-based journal reporting reveals that 96 percent of skilled nursing facilities did have an RN onsite for a minimum of 8 hours a day for 80 percent of the year however the weekend data reveal fared far worse. At 91 percent of the skilled nursing facilities, RN’s met federal guidelines less than 60 percent of the time. Generally, on the weekends, the overall staff was lower, including a reduction in licensed practical nurse (LPN) and nurse aide hours. On average, the worst staffing problems were found at larger skilled nursing facilities over the weekends. Higher rated (five stars) facilities that support fewer Medicaid residents had smaller fluctuations in staffing numbers.
Certified staff hiring and retention are longtime problems experienced by provider organizations. Recruiting and pay scales have been industry-wide challenges for years and are projected to get worse as the silver tsunami of baby boomers continues to stress available skilled nursing facility care. There is also a proposed change by CMS in how low-wage hospitals can pay employees, and this proposal will further stress the recruitment and retention process of nursing homes. The proposal, set to take effect in 2020, will address the bottom quarter of the pay index to increase wages at hospitals but does not provide a similar proposal to include skilled nursing facilities. The clear solution is to pay higher rates to caregivers, but these costs will be passed along to the resident consumer of the facility. However, for nursing homes with higher numbers of Medicaid residents, higher staff pay is an untenable solution.
While it is essential for skilled nursing facilities to meet CMS federal guidelines for RN staffing, the American Health Care Association (AHCA) is cautioning against viewing staffing numbers in a vacuum. “While staffing levels are one of many important metrics in quality care, judging the quality of a nursing home based solely on staffing is misguided,” said Courtney Bishnoi, Vice President of Quality and Programs at AHCA. “There is no question that the long-term care profession, along with health care providers across the spectrum, are facing a crisis…. AHCA is working with lawmakers to share policy that will help increase the number of workers.”
How you will be able to assess accurately and pay for skilled nursing facility care should the need arise is currently mired in change. Social programs like Medicare and Medicaid set standards; however, most of the facilities only meet federal guidelines part of the time. More expensive facilities seem to have better staffing records, yet the system assessment is guided by self-reporting by the facilities themselves to government entities. We can help you assess your situation, in particular how to finance your care in the future. Give us a call – we look forward to helping you and your loved ones achieve peace of mind.
Hermon Office: (207) 848-5600
Belfast Office: (207) 218-1599




